What’s MACRA
In 2015, the Medicare Access and CHIP Reauthorization Act (MACRA) became law. The buildup to MACRA seemed inevitable in the face of skyrocketing fees for healthcare.
MACRA would create a new approach in terms of delivering better, higher quality medical care while actually expending fewer resources in the process. Better care, more efficiently delivered? That’s Value-Based (VB), quality vs. quantity medicine … not fee-for-service medicine.
By operating under a VB medicine approach, CMS has calculated that billions of dollars would be saved by having physicians (aka, “Eligible Clinicians” or ECs) focusing on quality of care rather than quantity of care.
MACRA: Off the bat, MACRA replaced the Sustainable Growth Rate (SGR) formula which itself had been an ongoing issue for years.
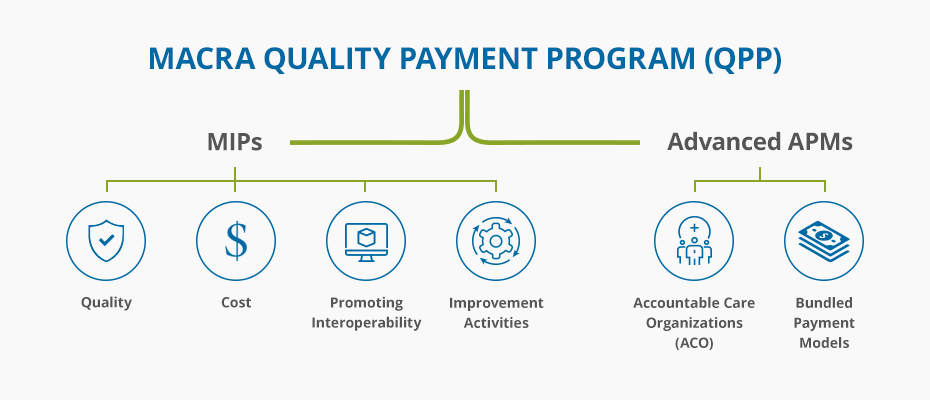
There are many aspects to MACRA, one of which is the Quality Payment Program (QPP). It’s the QPP segment that covers the two major tracks that ECs can follow for embracing VB medicine:
- MIPS (the Merit-based Incentive Payment System), and
- APSMs (Alternative Payment Models or advanced Alternative Payment Models); EPs who are in certain accountable care organizations (ACOs) would operate and report under the APM segment.
For MIPS, 2017 had its own reporting nuances including options on the length of time an EP could’ve chosen to report, from up to the entire 12 months in 2017 to lesser options that wouldn’t necessarily result in getting Medicare incentives, but would at least avoid Medicare penalties.
The up-to-4% penalty/incentive (or downward/upward adjustment) will be calculated against 2019’s Medicare reimbursements for 2017 reporting.
ECs always had the option to simply not participate and get penalized up to 4% by Medicare in 2019. Of course, they’d have no chance at getting any Medicare incentives.
APM: ECs operating under the APM scenario in 2017 will obtain a 5% lump sum bonus on their 2019 Medicare reimbursements based on the amount of money calculated as saved overall by the ACO for operating in a VB way vs. what would’ve expended on those same patients / diagnoses / procedures in a fee-for-service environment.
For 2018, things are a little different with MIPS and APMs, although one thing that’s the same is that a certified ERH is needed for reporting.
The EHR can be a 2014 or 2015 Edition CEHRT with 2015 adding an additional bonus of 10% on the incentive side.
Here are some bullets on what’s new for 2018:
- 2018’S reporting will produce any penalties or incentives against 2020’s Medicare reimbursements
- Those reimbursements will be positively or negatively impacted by up to 5%, with additional bonuses possible
- ECs who didn’t report at all in 2017 can report in 2018
- 2018 can be a full calendar reporting year if maximum incentives are being sought’, but it can also be a partial reporting year both time-wise and measures-wise just to avoid penalties
- ECs for 2018 are MDs, DOs, DPMs, DCs (as may be applicable per state), ODs, DDSs, DDMs, Pas, NPs, CNSs, and CRNAS
- ECs are exempt from 2018 reporting and will not be penalized by Medicare in 2020 if :
- they’re newly enrolled in Medicare during the 2018 performance period (exemption applies until the 2019 reporting period)
- their 2018 Medicare Part B charges are equal to or less than $90,000 / year or they see fewer than 200 Medicare Part B patients per year
- they’re significantly participating in Advanced APMs by receiving 25% of their 2018 Medicare payments through it, or they see 20% of their 2018 Medicare patients through an Advanced APM
- Non- patient – facing (NPF) ECs (radiologists, pathologist, etc.) who have up to 100 patient- facing encounters per year, or groups who have more than 75% of their NPIs billing under the group’s TIN during a performance period who are considered NPF
- Virtual groups are also considered NPF if more than 75% of NPIs within a virtual group during a performance period are non-patient facing
Unless you’re exempt, you must report at least minimally in 2018 or be ready for the negative impact against your 2020 Medicare reimbursements as previously described.
For 2018 MIPS, some familiar terminology has been reclassified for two of the four reporting categories, with “Meaningful Use” now being “Advancing Care Information” (ACI) and with the “Physician Quality Reporting System (PQRS) now being “Quality”.
The two other categories of reporting are Clinical Practice Improvement Activities (CPIA) and Cost.
Each of these components have details specific to them, and have their own reporting weight:
- Quality is weighted at 50% vs. 60% in 2017
- ACI (formerly “MU”) is 25%
- CPIA is 15%
- Cost is 10%, but EPs will not be responsible for additional reporting on cost
Ongoing penalties and incentives will rise annually over the ensuing years with 2019 reflecting against 2021’s Medicare reimbursements, 2020 against 2022, etc.
They’ll level off at up to penalties of 9% and remain at that rate in perpetuity for ECs who do not successfully report.
Simply stated, ECs will be Medicare – penalized for as many years as reporting isn’t done.
Registries and PTNs: The EHR vendor should have affiliations or collaborations with practice transformation networks (PTNs) and registries.
PTNs work with practices to help transform them from fee-for-service to VB, often at no cost or at a very nominal cost, and registries are great resources for reporting.
Visit www.cms.gov or www.qpp.cms.gov for more information. Your medical or specialty societies and practice administrator organizations no doubt have MACRA resources available to their members as well.
The bottom line is, if you’re an EC and you’re not exempt, you should definitely be in a VB medicine / MACRA frame of mind!
Your certified EHR should have a built-in MACRA DASHBOARD for compiling your reporting data. And your EHR vendor should have PTN and registry affiliations as wells as their own in-house MACRA TEAM to assist its clients.
Advanced Data Systems (ADS) is a vendor with those affiliations, and it has its Own MACRA team working closely with our clients.
Our Medics EHR IS 2015 certified and it contains a built-in MACRA dashboard allowing EPS to easily track their progress.
Incorporate Chronic Care Management (CCM) and Transition Care Management (TCM).
Reference/ source:
advanced data systems